What is Shigella?
Classification/Characteristics, Location, Gram Stain
What is Shigella?
First discovered in 1896 by Kiyoshi Shiga, a Japanese microbiologist, Shigella is a genus consisting of Gram-negative bacteria that cause bacterial diarrhea in human beings and some primates.
Members of this group are suggested to have evolved between 35,000 and about 170,000 years ago which makes them some of the earliest human pathogens. They can be found all across the globe and are responsible for between 5 and 15 percent of all cases of diarrhea (about 165 million cases of dysentery).
All members of this group are rod-shaped and non-motile. While they are also non-capsulated, Shigella species have been shown to be capable of surviving harsh conditions like freezing and relatively high pH levels. However, they can be easily destroyed through heat treatments.
The genus Shigella consists of four serological groups that include:
- Shigella dysenteriae (Group A and consists of 15 serotypes)
- Shigella flexneri (Group B and consists of 6 serotypes)
- Shigella boydii (Group C and consists of 18 serotypes)
- Shigella sonnei (Group D and consists of 1 serotype)
Classification
· Kingdom: Bacteria - Single-celled prokaryotes
· Phylum: Proteobacteria - Gram-negative bacteria most of which are pathogenic in nature. Some of the species are part of the normal human microbiota while others are free-living.
· Class: Gammaproteobacteria - Gram-negative bacteria, most of which are rod-shaped. While a good number of species in this group are pathogenic, others, like purple sulfur bacteria use light energy to produce organic molecules.
· Order: Enterobacterales - Members of this group are rod-shaped Gram-negative bacteria. They are also non-spore-forming and exist as facultative anaerobes.
· Family: Enterobacteriaceae - Rod-shaped Gram-negative bacteria that are non-motile and non-spore-forming. They are also facultative anaerobic bacteria with most of the species being pathogenic.
· Genus: Shigella
Characteristics of the genus Shigella are described below:
Characteristics of Shigella
Structure and Morphology
Shigella species are small single-celled organisms with a rod-shaped morphology. Depending on the species, they may range between 1 and 6um in length and 0.3 to 1um in diameter. Shigella dysenteriae, for instance, may range from 2 to 4um in length and 0.4 to 0.6um in diameter.
Like many other Gram-negative bacteria, Shigella species have an inner and outer membrane with a single layer of peptidoglycan separating the two. While the two membranes consist of a lipid bilayer, the outer membrane tends to be asymmetrical and is characterized by lipopolysaccharide (LPS) molecules and other proteins.
The inner membrane, on the other hand, is mostly composed of phospholipids like many other cell membranes.
* Shigella species have the O antigen in their lipopolysaccharide. This is an important component of the LPS that serves as the basis for the subdivision of Shigella serotypes. The O antigen consists of O units (oligosaccharide repeating units) which in turn contain between two (2) and eight (8) residues of broad range sugars
As is the case with many other Gram-negative bacteria, Shigella species also have a thin cell wall that consists of a single peptidoglycan layer. This layer consists of N-acetylglucosamine and N-acetylmuramic acid. Because of the thickness of the peptidoglycan layer (which is thin), Shigella cells cannot retain the primary stain during Gram staining.
* Shigella species are non-capsulated and therefore lack the polysaccharide layer that surrounds the cell envelop in some bacteria.
As prokaryotes, Shigella has a very simple structure when compared to eukaryotic cells - They lack membrane-bound organelles. However, they have a number of important organelles including ribosome and genetic material in the form of a single circular chromosome as well as a plasmid.
Characteristics of the Four Serological Groups
As mentioned, the genus Shigella is divided into four major serological groups.
As members of the Genus Shigella, the four groups have a number of similarities including the fact that they are all Gram-negative and are non-motile, etc. However, they also have a number of differences which makes it possible to distinguish them from each other.
Based on physiology, studies have shown serogroups A, B, and C to be very similar. For this reason, positive β-D-galactosidase and ornithine decarboxylase reactions are used to differentiate S. sonnei (serogroup D) from the other groups.
The majority of Group B, C, and D serotypes can be identified by their ability to ferment mannitol. This test can therefore be used to differentiate Shigella flexneri, Shigella boydii, and Shigella Sonnei from Shigella dysenteriae.
Some of the other characteristics used to differentiate between the four serogroups include:
· With the exception of serogroup D (Shigella sonnei), all the other serogroups are Ornithine decarboxylase (ODC) negative
· All the serogroups (with the exception of Shigella sonnei) do not ferment lactose and sucrose
· Ferment glucose without gas production
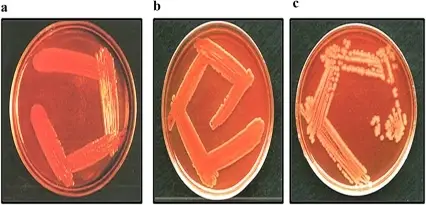
Identification of Shigella Species:
Agglutination Test
Apart from some of the characteristics described above, Shigella species can be identified using polyvalent Shigella antiser. Essentially, this test involves mixing the bacteria with an antiserum that contains specific Shigella antibodies.
Here, the bacteria will clump together in the presence of homologous antiserum which allows for the identification of the species.
The following are some of the steps involved in this procedure:
· Using a dropper, place two separate drops of saline on a clean glass slide - Make sure there is some distance between the two drops
· Using a sterile wire loop, obtain and emulsify a colony of the bacteria from culture with the two drops of saline to make a smooth suspension - This simply involves mixing the bacteria colony with the two salines (independent of each other) to make a smooth suspension
· To one of the suspensions (used as control) add a drop of saline and mix
· To the second suspension, add a drop of the antiserum and mix
· For about a minute, gently rock the slide back and forth and check whether agglutination occurs
* If agglutination occurs in the second suspension (the one to which antiserum was added), then it's possible to identify the species depending on the antiserum used.
Where is Shigella Found?
Shigella species are not commonly found living freely in the environment. However, they are facultative intracellular parasites and can therefore survive outside the host's body. Once they are released into the environment (along with fecal matter), Shigella species can survive without a host for about 50 days.
Apart from fecal matter and sewage, they can also be found in contaminated water sources and food material. For this reason, an individual can be infected if they ingest contaminated food material or drink contaminated water.
According to studies, foods that require a lot of handling during preparation are the ones that are more likely to be contaminated. These include potatoes, milk, and cheese, chicken, fish, and salads among others. While both contaminated water and foods can be the source of infections, foodborne Shigella infections are more common according to public health data.
With regards to distribution, Shigella species can be found throughout the globe. Some species are more abundant in certain regions than others. For instance, Shigella dysenteriae (serogroup A) which consists of 15 serotypes is commonly found in parts of Africa, Central America as well as the Indian subcontinent.
In these regions, the bacteria Type 1 Shigella dysenteriae has been associated with deadly epidemics if not controlled. Serogroup B (Shigella flexneri), as well, is commonly found in most developing nations. In these regions, however, the species causes less severe dysentery as compared to Shigella dysenteriae.
As compared to serogroup A, serogroup C (Shigella boydii) is commonly found in the Indian subcontinent and rarely in industrialized nations. Lastly, the serotype D is common in most developed nations but the infections are generally mild.
* Flies also play an important role in the transmission of the bacteria from fecal matter to food material or drinking water.
Infection
Shigella infection is known as shigellosis and is common worldwide. In third world countries, these infections have been associated with a relatively high mortality rate compared to outbreaks in developed nations particularly among children.
As mentioned, Shigella species can survive in the environment for a given period of time. An infection, therefore, occurs when an individual ingests contaminated food (particularly raw or fresh vegetables, chicken, and bakery products, etc) or drinks contaminated water.
An infection may result from soiled fingers of an individual (e.g. patient or child, etc) or following transfer by flies that have been breeding on contaminated feces. For this reason, it's important to thoroughly cook foods, wash hands with soap and water, and properly clean fruits and vegetables in order to control the spread of this infection.
Apart from the fecal-oral route of transmission, studies have shown infections to occur through oral-anal contact.
* These infections have also been observed among gorillas as well as some monkeys. However, this has only been shown to be the case in areas when these primates are in close proximity with human beings and not in the wild.
Following ingestion, Shigella is, for the most part, able to survive acidic conditions of the stomach which is one of the main adaptations of the bacteria. In order to establish a productive or successful infection, the bacteria have to invade colonic epithelial cells and then spread to other cells.
Before they actually invade the epithelial cells lining the large intestine, Shigella bacteria are first taken up by specialized epithelial cells of the small intestine known as Microfold cells (M cells).
Located in the gut-associated lymphoid tissue of the Peyer's patches in the small intestine, M cells play an important role in taking up microbial antigens in the intestine and taking them to the gut-associated lymphoid tissue (GALT) and then elicit an immune response.
In the gut-associated lymphoid tissue, these bacteria are engulfed by macrophages. In the macrophage, the bacteria disrupt the phagosome vacuole where it's contained and moves into the cytosol where it proliferates and consequently causes the death of these cells.
Even before Shigella is released from the dying macrophages, studies have shown Shigella cells to start releasing T3SS effectors that are involved in cell invasion. However, before they invade the epithelial cells of the large intestine, they first adhere to these cells (at the basolateral surface of epithelial cells) using IcsA (Shigella surface proteins) which acts as an adhesin.
Following attachment of these cells to the host cells, they activate their own internalization into the cells through the production of type III secretion system (T3SS).
In the host cells (epithelial cells of the large intestine), Shigella continue multiplying and increasing in numbers. In the process, they cause damage to the DNA as well as mitochondrial damage which triggers necrosis and apoptosis-associated death.
To spread from the basolateral side of the cell into the submucosa of the colon, Shigella moves from one cell to another through a process known as Paracytophagy. This is an actin-based motility that involves the utilization of host cell actin machinery for the parasite to move from one cell to another.
Here, Shigella surface proteins (IcsA) first interact with neuronal Wiskott - Aldrich syndrome protein and activate it. In turn, neuronal Wiskott - Aldrich syndrome protein recruits a seven-subunit protein complex known as Arp2/3 which is involved in actin polymerization.
Actin produced here promotes Shigella motility from one cell to another through the formation of protrusions in the membrane of the host cells.
* As compared to some of the other pathogens that cause diarrhea in human beings, Shigella is highly contagious and only a few individual cells (about 200) are required to cause a successful infection.
Shigella Toxin
In addition to invading cells and affecting various cell processes, Shigella bacteria produce toxins that impact cell functions. The lipopolysaccharide of Shigella (located on the outer membrane), consists of lipid A and has been shown to exhibit endotoxic activities.
This heat-stable toxin has been shown to cause a fever following a successful infection by the bacteria. Generally, the endotoxin is not highly specific and has a relatively low degree of potency. Regardless, it causes fever which is one of the symptoms of the infection.
Apart from the endotoxin, Shigella also produces an exotoxin known as Shiga toxin. One of the most common Shiga toxin is the Shiga toxin (Stx) produced by Shigella dysenteriae 1. However, some of the other Shigella species have also been shown to produce these toxins.
For instance, Shigella flexneri produces Stx 1. As compared to the endotoxin, the exotoxin is extremely potent and inhibits protein synthesis by infected cells. Moreover, it consists of enzymatic and binding subunits that enhance its functions.
While the binding component of the toxin allows it to bind to target cells, the enzymatic components contribute to its entry into the cell.
Among infected individuals, Shiga toxin has the following effects:
Enterotoxin effect - As an enterotoxin, Shiga toxin blocks the absorption of various substances (glucose, amino acids, and electrolytes, etc) by epithelial cells of the intestine lumen. They achieve this by adhering to the intestine receptors thereby preventing absorption - In the process, this also results in fluid accumulation because absorption is inhibited.
Cytotoxic effects - In the large intestine, the binding subunit of the toxin (B subunits) binds to the glycolipid located in the host cell. This is followed by entry of the enzymatic subunit that inactivates the 60S ribosome subunit thus affecting protein synthesis. By inhibiting protein synthesis, the toxin causes the cells to die.
Neurotoxic effect - Neurotoxic effects of Shiga toxin involves blocking nerve impulses. Consequently, this contributes to paralysis. Some of the signs of neurotoxicity include fever and abdominal cramping.
* The Shigella bacteria is released into the environment during defecation and the cycle continues when the fecal matter contaminates drinking water or food material.
Symptoms
Usually, patients start presenting symptoms of shigellosis 3 days following the initial contact with the pathogen. However, in some cases, this may occur one week after contact.
One of the most common symptoms of shigellosis is watery diarrhea which may be associated with vomiting and moderate dehydration. As mentioned, one of the effects of Shigella toxin is that it prevents the absorption of various substances which in turn results in fluid accumulation.
In the process, this contributes to watery diarrhea. Apart from watery diarrhea, dysentery is the other clinical presentation of this infection. This may also be characterized by a mucoid and slightly bloody stool.
Some of the other symptoms of shigellosis may include:
- Abdominal cramping
- Nausea
- Fever
- Stomach tenderness
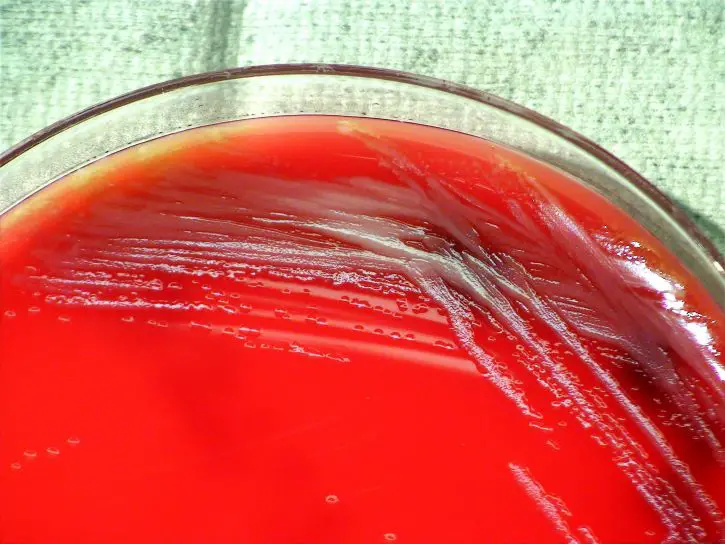
Gram Stain
Requirements
- Sample - Samples that can be used include stool mucus, stool or a colony sample from culture
- Gram stain reagents
- Staining rack
- Glass slide
- Water
- Heat
- Bunsen burner
- Wire loop
Procedure
· Using a sterile wire loop, obtain a small amount of the sample and create a thin smear on a clean glass slide - It's always important to ensure that the slide and wire loop are both sterile in order to prevent contamination.
· Carefully pass the slide over the Bunsen burner flame to heat fix - The slide can be passed over the flame about 3 times while avoiding overheating.
· Allow the slide to air dry and then flood with crystal violet for about 1 minute.
· Gently wash the slide with a running stream of water (about 2 seconds).
· Flood the slide with Gram's iodine (mordant) and allow it to stand for about 1 minute.
· Again gently wash the slide with a running stream of water (about 2 seconds).
· Add a few drops (drop by drop) of the decolorizing agent (95% ethyl alcohol or acetone) until it runs clear.
· Flood the slide with the counterstain/secondary stain (e.g. Safranin) and allow to stand for about 1 minute
· Gently wash the slide in a stream of running water.
· Observe the slide under oil immersion.
Observation
When viewed under the microscope, Shigella species will appear as rods that may range between 1 and 6um in length depending on the species. They are also pink reddish in color given that they take up the color of the counterstain.
Difference between Shigella and Salmonella
Salmonella and Shigella (members of the family Enterobacteriaceae) are some of the most common causes of bacterial foodborne diseases in different parts of the world.
Although they have several similarities (e.g. they are both rod-shaped, Gram-negative bacteria), the two types of bacteria have a number of differences that can be used to distinguish between them.
These include:
Motility - Unlike Salmonella which has several flagella used for adhesion, forming a biofilm, and movement, Shigella do not have this structure. For this reason, they are often described as being non-motile.
Acid resistance - Following ingestion of Shigella, studies have shown the bacteria to be more resistant to gastric acid when compared to some of the other intestinal bacteria (Salmonella, etc). This has been attributed to the expression of proteins like GadA/B that allow the bacteria to survive long enough to invade intestinal cells.
Because Salmonella is not resistant to gastric acid, the bacteria has been shown to depend on food material for their survival as well as lowering their own pH.
Infection dose - In shigellosis, only a small number of bacterial cells are required to cause an infection (about 200 cells). However, a large inoculum of Salmonella is required for an infection to occur. For instance, at least 100000 Salmonella typhi cells are required to cause typhoid.
Hydrogen sulfide - Unlike Shigella, Salmonella (S. enterica) produce hydrogen sulfide which is one of the characteristics used for their identification.
Infection - Shigella primarily affects the large intestine while Salmonella affects both the small and large intestine.
Disease - Whereas Shigella causes Shigellosis in human beings and some primates, Salmonella causes Salmonellosis in human beings and some animals. Here, however, the symptoms may be similar (E.g. Fever, diarrhea, and abdominal pain, etc).
* While both Salmonella and Shigella are both rod-shaped, Shigella species are generally slender (0.3 to 1um in diameter) compared to Salmonella which range between 0.7 and 1.5um in diameter. Moreover, Shigella only has fimbriae on their surface while Salmonella have both fimbriae and flagella on their surface.
Return to Bacteria main page, Eubacteria
Return from Shigella to MicroscopeMaster home
References
Arun Bhunia. (2007). Foodborne Microbial Pathogens: Mechanisms and Pathogenesis.
Ewing. W.H. (1986). Edwards & Ewing’s Identification of Enterobacteriaceae. 4th edition.
Hiroshi Ashida, Minsoo Kim, and Chihiro Sasakawa. (2014). Manipulation of the host cell death pathway by Shigella.
Lu Feng et al. (2004). Structural and Genetic Characterization of the Shigella boydii Type 13 O Antigen.
Public Heath England. (2015). UK Standards for Microbiology Investigations
Identification of Shigella species.
Links
https://www.healthline.com/health/shigellosis
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/shigella
Find out how to advertise on MicroscopeMaster!