Immunohistochemistry and Microscopy
Techniques - Cancer Research
For little less than a century, scientists have been utilizing immunohistochemistry techniques to study, identify, and diagnose a variety of antigens that are present in diseased tissue, as well as those that cause an infection.
This 83 year-old process is so important that laboratories all over the world, whether they specialize in research or diagnostics, consider the technology to perform this study, as well as the trained and experienced scientists knowledgeable enough to perform the techniques, a basic necessity.
The progress made in this area of study also makes it a primary tool in diagnosing different types of cancer, determining if a tumor is benign or malignant and identifying its stage, grade and place of origin.
Defining Immunohistochemistry
This big word may seem intimidating but if you break it down into pieces, such as “histo”, which means tissue, and “immune”, which pertains to treatments of the immune system, you can obtain a general understanding of what this area of science studies.
Still, the actual definition of immunohistochemistry is a bit more detailed, as it is not simply the study of the tissue’s immune system but rather, a study of the immune’s system response to infected tissue and the chemistry that causes a particular reaction.
When stimulated by a foreign substance, the immune system secretes antibodies, or proteins, as a defense mechanism to keep your body safe and healthy. The foreign bodies, otherwise known as antigens, which are also typically proteins, stimulate the immune system, causing it to generate antibodies.
Antibodies and antigens work like a lock and a key, for each specific lock, you have a specific key. When a particular antigen invades your body, the corresponding antibody binds to it with the goal of destroying it, thus preventing it from reproducing, spreading and causing you further harm.
The discovery of these facts lead to the conception of immunohistochemistry, as the technique mimics the body’s natural process in a lab setting, allowing scientists to study the particular antibodies generated in a specific piece of organ tissue that the immune system automatically released to fight the specific invading antigens.
In doing so, researchers can determine the treatments that respond the best to a specific antigen, as well as those that have no effect, allowing for the creation of new antibiotics and other medicines that imitate the body’s natural response to an invader.
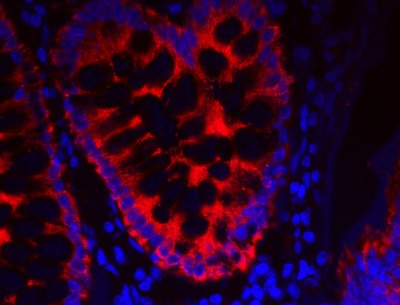
Fluorescent IHC detection of cytokeratin 18 in colon carcinoma tissue
Image: Piercenet.com - Thermo Scientific Pierce Protein Biology Products
Technique
Immunohistochemistry involves many steps, is time consuming and the slightest mistake or touch of a contaminant can ruin the sample, giving the scientist not choice but to start the process all over again with a new specimen.
To start, a doctor or technician collects a tissue sample by either performing a biopsy, obtaining a piece of the organ in question, such as the liver, or by taking the whole specimen, for instance a single kidney.
The sample then needs to go through the process of fixation, a method of preservation that almost always includes the use of formaldehyde.
Cryogenic Embedding
Next, the scientist must embed the specimen into a casing to preserve the natural structure of the tissue sample. This is sometimes more involved, as in the case of cryogenic embedding and snap freezing with the use of liquid nitrogen.
Once the sample is set, the researcher then has to divide the tissue into sections, mount and adhere it onto the slide, dry it and then prepare it for deparaffinization.
In the cases that involve cryogenic embedding and freezing, the sectioning, mounting, drying and preparation techniques differ from those of non-frozen tissue samples.
Binding and Blocking
After preparing the specimen, the scientist must remove the adherent from the sample so that the antibody involved in the particular study has the ability to bind to the corresponding antigen.
The researchers may also have to add blockers to other protein sites on the sample to prevent false results, as antibodies sometimes form weak attachments to reactive sites that are not part of the antigens.
Additional Steps
Now that the sample is ready, more steps need to occur to conduct tests, obtain results and analyze the collected data. To perform their research, scientist must treat the tissue with the antibodies that correspond with the particular antigens.
In order to view the reactions under a fluorescence microscope, the addition of a fluorescent dye, a radioisotope, colloidal gold or other color differentiating stain is necessary.
In some tissues, autofluorescence or natural fluorescence exists. When fluorescent dyes are added, this results in imaging background problems. Before antibody incubation, testing for autofluorescence in tissues can be done with a fluorescence microscope. Then one is able to determine that avoidance of the fluorescent technique will be necessary and choose enzyme or other labeling techniques instead.
Once the scientist properly completes all of the immunohistochemistry processes, he or she can move on to observing the sample and documenting the results.
Cancer Research
One area of medicine in which immunohistochemistry is predominantly used is in identifying particular types of cancer, its point of origin and its current level of growth.
A scientist can choose from one or more of hundreds of different types of antibodies to use for testing, some of which react with various types of cancers while others only bind to antigens found in a specific type of cancer.
This information is crucial for doctors because it allows them to decide what treatment options are available based on the diagnosis and if there are any risk factors, as immunohistochemistry also tests for infections, which are common in cancer patients.
Another important reason scientists conduct immunohistochemistry tests with regards to cancer is because instances sometimes occur in which a person appears to have cancer, or cancer-like symptoms, but they in fact have an infection that is not at all cancerous.
Medical professionals most commonly perform tests of this nature in cases that pertain to the lymphatic system, as the lymph nodes often swell in the presence of an infection but can also form a noticeable mass in the event of a tumor.
Immunohistochemistry is an amazing scientific technique that involves many steps, each one crucial to the accuracy of the overall test results, as a single false result could cost someone their health, or even their life.
Fortunately, scientists often perform these tests more than once and they observe multiple specimens from different pieces of the tissue sample, thus ensuring results free from errors.
Though an old-standing method of testing, this process has seen improvements and it continues to be one of the most reliable diagnostic tools, particularly in cancer cases, used by modern scientists.
Understanding immunofluorescence applications and methods
Histochemistry - Techniques, Staining and Tests
Return from Immunohistochemistry in Microscopy to Fluorescence Microscope
Return to MicroscopeMaster Home
Find out how to advertise on MicroscopeMaster!