How Do Antibiotics Kill Bacteria?
What are Antibiotics?
Antibiotics are compounds used for the purposes of treating infections caused by bacteria. Depending on the type of antibiotic used or type of bacteria, these compounds achieve their function by either destroying the microorganism or simply stopping their proliferation (inhibiting reproduction).
While most antibiotics are natural compounds derived from plants and other living organisms, others are chemically produced based on the structure of natural compounds.
While a good number of antibiotics have been shown to affect the normal microbial flora, particularly in the gut, they do not affect normal, healthy cells because of the mechanism through which they treat an infection. Moreover, they are ineffective against viruses because of the differences in the general structure (between bacteria and viruses).
As mentioned, there are different sources of antibiotic compounds in nature which include:
- Algae: E.g. methanolic compounds produced by Tetraspora cylindrica (green algae)
- Lichens: E.g. Usnic acid (a dibenzofuran derivative)
- Fungi: E.g. penicillin produced by
- Actinomycetes: e.g. tetracyclines, macrolide, streptomycin
- Certain plants: E.g. polyphenols and some alkaloids
- Some bacteria: E.g. polymyxin B produced b Bacillus polymyxa and bacitracin produced by Bacillus subtilis
* Some antibiotics can be used against fungal infection and some microorganisms. For instance, polyenes are used against some fungal infections
* Antibiotics may be classified as broad-spectrum antibiotics such as quinolones and cephalosporins which act against a wide range of microorganisms/bacteria, or narrow-spectrum antibiotics (e.g. fidaxomicin and vancomycin etc) which only act against a few species of bacteria.
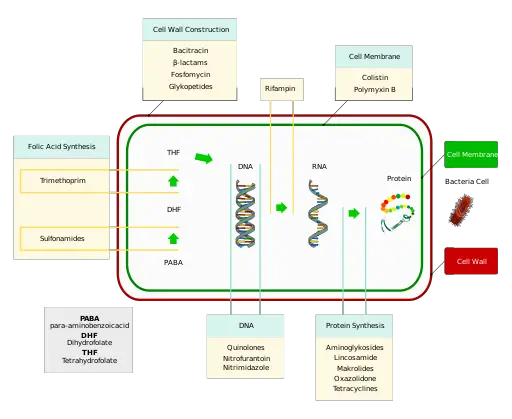
Mode of Action
As mentioned, different types of antibiotics treat bacterial infections through different mechanisms. Whereas some of the antibiotics act by completely destroying the microorganism, others slow or stop their growth/reproduction thereby preventing the infection from spreading.
Here, antibiotics that kill/destroy the bacteria are known as bactericidal antibiotics while those that inhibit growth/reproduction are known as bacteriostatic antibiotics.
The following section will look at some mechanisms behind the action of bactericidal and bacteriostatic antibiotics:
Bacteriostatic Antibiotics
Protein-synthesis inhibitors
Protein-synthesis inhibitors are examples of bacteriostatic antibiotics. As such, they act by slowing or stopping the growth of bacterial cells during treatment. While this action does not immediately kill bacteria, it prevents them from growing thus causing them to die without reproducing.
Some good examples of protein-synthesis inhibitors include macrolides like erythromycin. Depending on the type of antibiotic used, protein-synthesis inhibitors may inhibit the synthesis of protein in a number of ways.
These include:
- Interfering with the elongation of the peptide chain
- Inhibiting ologosaccharide side chains from attaching to glycoproteins
- Causing the misreading of genetic information or blocking the A site of ribosome (ribosome are involved in protein synthesis).
While there are several ways through which these antibiotics can interfere with protein synthesis, this is generally at the ribosomal level. This means that they act by affecting the functions of the ribosome in protein synthesis.
For proteins to be synthesized, then the information contained in the messenger RNA has to be translated. This process is known as translation and results in the production of proteins following the assembly of amino acids. The ribosome, which is involved in protein synthesis, consists of three binding sites (A, P, and E) involved in the elongation of the peptide chain.
When a protein-synthesis inhibitor like aminoglycosides binds to a site adjacent to the decoding site of the ribosome (in the 30s subunit), it directly interrupts initiation of protein synthesis by causing the misreading of the genetic information. This prevents the elongation of the peptide chain thus preventing protein synthesis.
For some bacteria, especially some aerobic gram-negative bacilli, this activity has been shown to be bactericidal. However, for many other bacteria, this may affect growth or reproduction thus preventing proliferation.
Nucleic acid synthesis inhibitors
While Nucleic acid synthesis inhibitors can cause the death of some bacterial cells (bactericidal activity), they are generally classified as bacteriostatic antibiotics. They include such antibiotics as quinolones, rifamycins, and metronidazole, etc.
As the name suggests, these antibiotics function by interrupting the synthesis of DNA especially during DNA replication. For different antibiotics, however, this is achieved through different mechanisms.
Some of the most common mechanisms include:
Breakage of DNA strand - Some antibiotics function by causing the DNA strand to break down which in turn affects other cell processes. In the case of antibiotics like Metronidazole, they first diffuse across the membrane to enter the cell (especially anaerobic bacteria).
In the cell, this compound is acted upon by the enzyme Pyruvate ferredoxin oxidoreductase (PFOR) which converts it into a nitro radical (nitro radical anion).
This form of the drug is highly reactive and while it attacks the DNA causing it to break down, it's also responsible for a concentration gradient that causes the uptake of more drug compounds into the cell.
Here, the cytotoxic effects of the drug can either directly destroy the cell or affect cell division thereby preventing proliferation.
See also: Cytotoxicity testing
Inhibiting DNA replication and cell growth - Unlike antibiotics that cause the DNA strand to break down, some antibiotics act by inhibiting DNA replication and cell growth. A good example of these antibiotics is quinolones (levofloxacin, ciprofloxacin, and moxifloxacin, etc).
In order to understand how these antibiotics work, it's worth noting that for DNA replication to occur, then tightly coiled chromosomes have to be unwound (so that the information can be copied), a function carried out by two important topoisomerases (topoisomerase IV and DNA gyrase).
To prevent this unwinding of the DNA, these antibiotics target and bind the two topoisomerases thus inhibiting DNA replication. By inhibiting DNA replication, this directly affects cell division as well as cell growth.
Interrupting transcription - Some antibiotics act by interrupting the transcription process. Essentially, transcription refers to the process through which information contained in the DNA is transferred to the mRNA which is in turn involved in translation.
Rifamycins are an example of antibiotics that act through this mechanism. The main transcription enzyme is known as RNA polymerase. Here, the enzyme uses a single DNA strand to produce a complementary RNA molecule involved in translation.
In order to stop transcription, the antibiotic attaches to the enzyme thus preventing it from performing its function. By inhibiting transcription, the mRNA required for translation is not produced. This affects various cellular processes which can in turn affect cell development, cell division, and cell death.
Bactericidal Antibiotics
While the antibiotics and mechanisms highlighted above affect cell division, cell growth, and even cell death in some cases, bactericidal antibiotics directly kill bacterial cells.
This section will focus on some of the mechanisms, as well as antibiotics, involved in the destruction of bacterial cells.
Cell Wall Synthesis Inhibitors
Antibiotics that interrupt the synthesis of the cell wall of bacteria act by disrupting synthesis of the peptidoglycan. In doing so, they cause the cell to be susceptible to mechanisms like osmotic lysis thus contributing to cell destruction.
For this reason, these inhibitors are classified as bactericidal antibiotics. Penicillins, which are some of the most common antibiotics, are examples of cell wall synthesis inhibitors.
Unlike most eukaryotic cells (especially in animals), bacteria have a cell wall that surrounds the cell membrane. This cell wall consists of alternating chains of linked N-acetylglucosamine and N-acetylmuramic acid with short peptide chains cross-linking them.
While some bacteria have several peptidoglycan layers (Gram positive bacteria) while others only have a single peptidoglycan layer, they are all characterized by the presence of a cell wall which serves a number of functions including maintaining the cell shape, protecting the cell, providing support, as well as controlling expansion of the cell, etc.
Here, synthesis of the peptidoglycan (a major component of the cell wall) is mediated by a number of factors including the transpeptidase enzyme. These enzymes are also capable of binding penicillin and are therefore also referred to as penicillin-binding proteins.
The B-lactam ring of penicillin binds (irreversibly) to the active site of the enzyme and reacts with the serine residue to the protein which in turn inhibits its action - action of the transpeptidase enzyme.
Because of the actions of the antibiotic, the bacterium is unable to fill the large pores with the peptidoglycan required to properly cover the cell. This is especially a big problem during cell division given synthesis of new peptidoglycan is inhibited following the separation of two cells.
As a result, water moves into the cell because the cells consist of a higher concentration of solutes, ultimately causing destruction of the cell through lysis (osmotic instability).
Membrane Disruptors
Whereas some antibiotics act by inhibiting synthesis of the peptidoglycan layer of growing and dividing bacteria, others function by disrupting the integrity of the cell membrane. This is an effective mechanism as the cell membrane is primarily involved in the movement of material in and out of the cell.
Some of the antibiotics commonly used here include daptomycin and polymyxins. Daptomycin will be used to explain the mode of action of these antibiotics.
Produced by Streptomyces roseosporus, a Gram-positive soil bacteria, Daptomycin is characterized by a total of 10 amino acid residues, three exocyclic amino acids as well as a decanoylfaty acid tail. Because the compound is negatively charged, studies have shown that it depends on the calcium ions on the surface of the cell to gain entry.
Here, the compounds first form a complex with the calcium ions (Ca2+–daptomycin complex) which has a lesser negative charge compared to the original compound.
In addition, the complex has a higher affinity for the membrane phospholipid (phospholipid phosphatidylglycerol) which are generally negatively charged because of the phosphate group.
Following aggregation of the compound on the membrane, studies have shown this to result in the formation of micelles (large pores) allowing for the leakage of potassium ions. In turn, this results in dissipation of membrane potential and consequently the death of the cell.
* Daptomycin is generally used to target the membrane of Gram-positive bacteria which lack an outer membrane.
Metabolic pathway Inhibitors
Antibiotics that act by targeting the metabolic pathway of bacteria are often referred to as antimetabolites. One of the reasons they are effective in inhibiting the metabolic pathway is because they have some similarities to the natural metabolites. However, their differences allow them to interfere with normal metabolism which in turn results in cell death.
One of the most popular metabolic pathway inhibitors is Trimethoprim. As an Antifolate, trimethoprim is used to interrupt the action of folic acid - a vitamin that is produced by bacteria for the synthesis of nucleic acid and proteins.
Trimethoprim acts by combining with dihydrofolate reductase which is the enzyme that serves to reduce dihydrofolic acid to tetrahydrofolic acid. In doing so, this antibiotic interrupts the pathway of folic acid synthesis and therefore directly inhibits the production of nucleic acids and proteins.
How do Antibiotics kill Bacteria without harming the Host?
Given that antibiotics function by targeting given sites of the bacterial cell or certain cellular processes, one may expect that they can also act against and damage cells of the host.
This is not the case for the following reasons:
Cell Wall/Peptidoglycan
As mentioned, the majority of bacteria have a cell wall (which consists of peptidoglycan) surrounding the inner membrane. This is an important component of these bacterial cells that is lacking in human beings and other animals.
When drugs like penicillin are used to treat the infection, they target and inhibit the enzymes involved in the synthesis of the cell wall/peptidoglycan and affect its function resulting in the destruction of the bacterial cell.
Given that animal cells do not have a cell wall or enzymes involved in the synthesis of this structure, the drugs cannot cause harm.
Cell Membrane
While some antibiotics act by targeting and destroying the cell wall, others function by targeting the cell membrane. Given that human beings and other animals also have a cell membrane, then host cells can also be targeted in the process.
Here, however, most of these antibiotics are used topically and therefore cannot cause significant damage. These antibiotics (e.g. mupirocin) are particularly effective against bacteria like Staphylococcus aureus responsible for skin infections.
Protein-synthesis Inhibitors
Drugs like tetracycline are used to disrupt bacterial growth by inhibiting protein synthesis. Like bacteria, human beings (eukaryotes) also have ribosomes that are involved in protein synthesis.
Whereas human ribosomes are larger and consist of the 60S and 40S subunits, bacterial ribosomes are small in size and consist of the 40S and 30S subunits.
Protein-synthesis inhibitors function by specifically targeting the 30S subunit of the bacterial ribosome and cannot affect protein synthesis in the host cells. The differences in the target ensure that host cells are not harmed.
Nucleic Acids Synthesis Inhibitors
As is the case with protein synthesis, there are differences in polymerases and other factors involved in the synthesis of nucleic acids between human beings (and other animals) and bacteria.
Here, then, antibiotics used to treat infections specifically target the factors involved in this synthesis in bacteria which allows them to only destroy or stop the growth of bacterial cells without causing harm to the host cells.
Bacteriology as a field of study
Bacterial Transformation, Conjugation
How do Bacteria cause Disease?
Bacteria - Size, Shape and Arrangement - Eubacteria
Does Salt Water kill Bacteria?
Which Bacteria cause Food Poisoning?
How Antibiotic Resistance happens and How to Prevent it
List of Diseases caused by Bacteria
Return from How do Antibiotics kill Bacteria? to MicroscopeMaster home
References
Deborah A. Williamson, Glen P. Carter and Benjamin P. Howden. (2017). Current and Emerging Topical Antibacterials and Antiseptics: Agents, Action, and Resistance Patterns.
Elena Martínez-Francés and Carlos Escudero-Oñate. (2018). Cyanobacteria and Microalgae in the Production of Valuable Bioactive Compounds.
Geisla Mary Silva et al. (2012). Mechanisms of action of systemic antibiotics used in periodontal treatment and mechanisms of bacterial resistance to these drugs.
William R. Miller, Arnold S. Bayer and Cesar A. Arias. (2016). Mechanism of Action and Resistance to Daptomycin in Staphylococcus aureus and Enterococci.
Links
https://ceufast.com/course/protein-synthesis-inhibitors
Find out how to advertise on MicroscopeMaster!