Hematopoietic Progenitor Cells (HPCs)
Meaning, Transplantation/Cell Markers
Proliferation
Meaning
Hematopoietic progenitor cells (HPCs) are cell types that develop from hematopoietic stem cells. As the name suggests, these cells give rise to one or more types of mature blood cells in the body.
Although the terms hematopoietic progenitor cells and hematopoietic stem cells are used interchangeably in some literature, it's worth noting that unlike stem cells, which can develop to any blood cell lines, progenitor cells (which are produced by stem cells) are limited and can only give rise to one of a few blood cells.
While some studies have suggested that hematopoietic stem cells are not just hematopoietic and thus capable of giving rise to other types of cells in the body as pluripotent cells, they are generally classified as multipotent cells that are only capable of giving rise to a family of closely related cells.
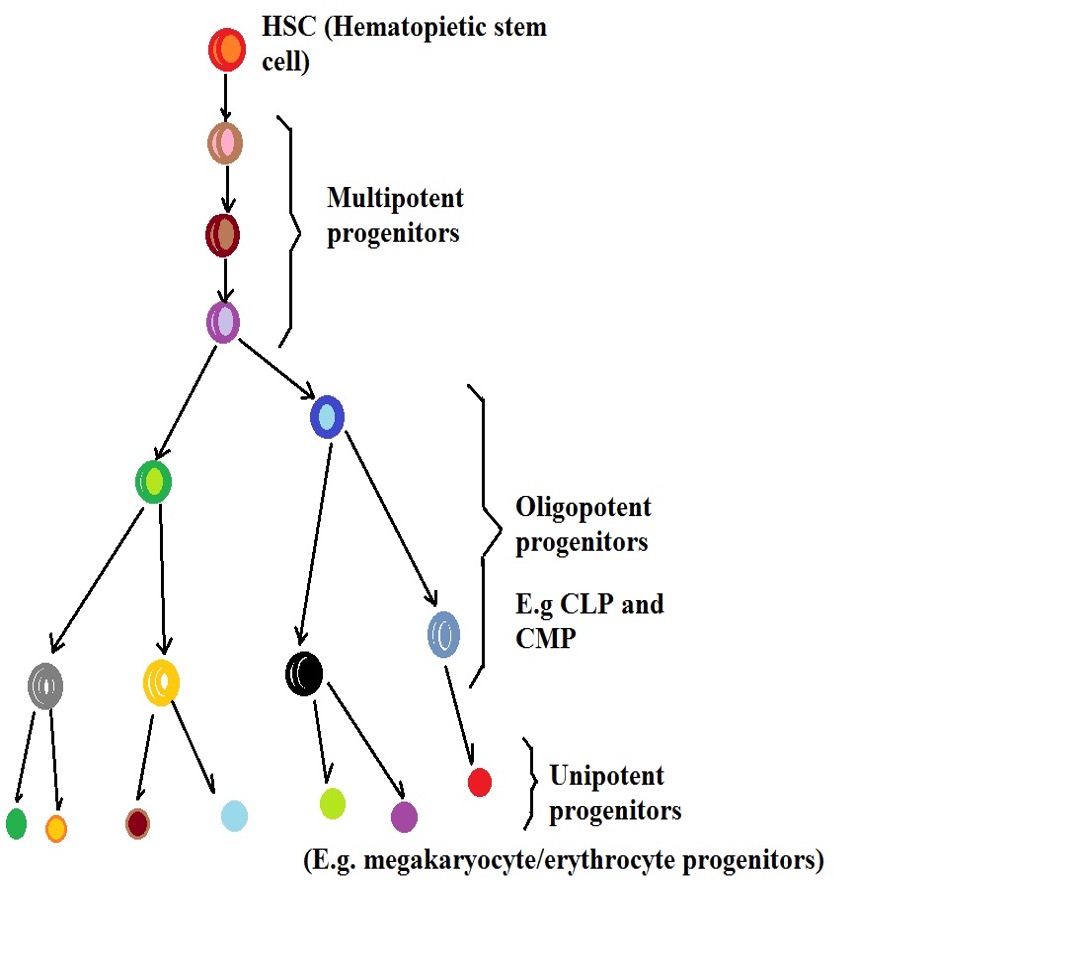
Here, the hematopoietic progenitor cells produced by hematopoietic stem cells are classified/categorized based on their potency.
These include:
· Multipotent hematopoietic progenitor cells - Cells that produce most subsets of blood cells
· Oligopotent hematopoietic progenitor cells - These include lymphoid and myeloid progenitor cells which are restricted to the two lineages
· Unipotent hematopoietic progenitor cells - Restricted to the production of one set of blood cells e.g. unipotent megakaryocytic progenitor cells
Proliferation
Generally, red blood cells have a short life span and therefore have to be renewed to maintain the normal number at all times. In the hematopoietic system, special cells known as hematopoietic stem cells remain at the top of the hematopoietic hierarchy and not only continually renew themselves, but also differentiate in order to emerge into different types of effector cells.
Before they can give rise to fully committed effector cells, hematopoietic stem cells first differentiate to produce progenitor cells that are more committed compared to the stem cells.
As compared to hematopoietic stem cells, hematopoietic progenitor cells which include multipotent, oligo-potent, and progenitor cells restricted to a single lineage, are more proliferative given that they are directly responsible for the renewal of the different types of blood cells.
Following the proliferation of hematopoietic stem cells, a single daughter cell resembling the parent and another that differentiates into a progenitor cell are produced.
Although the progenitor cells produced by hematopoietic stem cells turn into more differentiated cells, they are not capable of prolonged self-renewal. This is not really necessary given that stem cells continue to produce new progenitor cells when need be. This means that new progenitor cells are always being produced to maintain the normal numbers of effecter cells in the body.
Here, however, it's worth noting that this process is strictly regulated to keep the number of progenitors in check in order to prevent the development of such conditions as leukemia.
In the event of deregulation, the high proliferation and differentiation of hematopoietic stem cells and hematopoietic progenitors cause them to gradually transform into disease-initiating cells that can result in various malignancies.
Given that progenitor cells are, for the most part, incapable of prolonged self-renewal, this section will focus on rapid division/proliferation and the subsequent differentiation which gives rise to mode differentiated cells:
Multipotent Progenitor Cells
Multipotent progenitor cells are the immediate products of hematopoietic stem cells. Being some of the earliest cells produced in the hematopoietic system, multipotent progenitor cells are less differentiated compared to the other progenitor cells in this lineage. As such, they differentiate and give rise to a subset of various types of cells.
In both mice and human beings, studies have shown multipotent progenitors (hematopoietic multipotent progenitor cells) rapidly proliferate which in turn allows them to become oligopotent progenitors.
Here, division of the multipotent progenitors is important as it allows them to ultimately increase to the appropriate number of blood cells depending on the needs of the body (e.g. in the event of an infection etc). Here, however, the proliferation of these cells is important for differentiation rather than self-renewal.
Oligopotent Progenitors
Oligopotent progenitors are some of the most common hematopoietic progenitor cells and are the products of multipotent progenitors.
While there are several types of oligopotent progenitors including megakaryocyte–erythroid progenitor cell and granulocyte-monocyte progenitor which are classified as oligopotent progenitors, this section will primarily focus on common lymphoid progenitor cells (CLPs) and common myeloid progenitor cells (CMPs).
In human beings, studies have shown myeloid progenitors to undergo rapid proliferation before they differentiate to produce more functional cells (particularly macrophages and monocytes).
For the proliferation of myeloid progenitors to occur, given factors are required. For instance, when the body needs to produce an increased number of monocytes and macrophages, Macrophage Colony-Stimulating Factor (M-CSF) is produced which stimulates the proliferation of these cells.
The rapid proliferation of myeloid progenitors allows them to increase in number before they start differentiating to produce the functional/fully differentiated cells.
Like myeloid progenitors, lymphoid progenitor cells are also classified as oligopotent progenitors. These cells are responsible for the production of lymphocytes, dendritic, and natural killer cells.
A number of factors including IL-3, IL-5 and agranulocytic colony-stimulating factor (AG-CSF) influence the proliferation of these cells as well as their differentiation to produce the lymphoblast that in turn gives rise to the lymphocytes.
Like myeloid progenitors, these cells have to undergo rapid proliferation in order to increase in number followed by differentiation.
Factors such as IL-3 and 5 act as regulators and thus only activate increased proliferation when need be. Increased or decreased production of the stimulating factors therefore has a direct impact on the proliferation rate of lymphoid progenitors.
* Some examples of unipotent progenitors include the lymphoblast (produced by lymphoid progenitors) and megakaryoblast among others. Unlike the other progenitors, these cells are only capable of proliferating and differentiating to give rise to specific types of cells.
For instance, megakaryoblast gives rise to promegakaryocyte which in turn produces platelets.
Unlike multipotent and oligopotent progenitor cells, hematopoietic progenitor cells can only become a single set (a single type) of blood cells. This process is also regulated and requires the progenitor cells to receive signals for them to proliferate and differentiate.
The following are unipotent hematopoietic progenitor cells and the cells they produce after differentiation:
· Human Megakaryocyte Progenitors (MkP) - blood thrombocytes (also known as platelets)
· Erythroid progenitors: Erythrocytes
· Mast cell progenitors (MCP) - Give rise to mast cells
· Macrophage and dendritic cell progenitors (MDPs) - These progenitor cells give rise to macrophages and dendritic cells
· Eosinophil lineage-committed progenitors (EoPs) - give rise to eosinophil cells
· Granulocyte-monocyte progenitor (GMP) - gives rise to granulocytes
Hematopoietic Progenitor Cells Transplantation
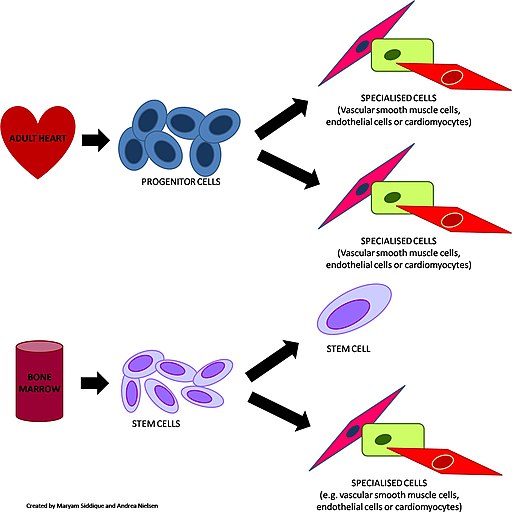
Essentially, the transplantation of hematopoietic progenitor cells involves using transplants (either autologous or allogeneic) to replace those of the recipient's bone marrow. This method has been used for the purposes of treating hematologic malignancies as well as certain solid tumors.
Given that hematopoietic progenitors (e.g. multipotent hematopoietic progenitor cells) can rapidly proliferate and differentiate to produce mature and functional blood and immune cells, this allows for the replenishment of normal and functional cells in the patient.
Based on a number of studies, researchers discovered that a given amount of hematopoietic stem and progenitor cells are capable of leaving the bone marrow. From the bone marrow, they can enter circulation and be transported to various tissues. Therefore, the cells can be easily obtained from the donor’s blood.
The donor is often given medication that helps move more stem or progenitor cells from the bone marrow into the bloodstream. This allows for a good number of the cells to be collected and infused into the patient.
The following are some of the main steps/stages involved in hematopoietic progenitor cells transplantation:
Step 1: Finding a donor
As mentioned, transplantation may be allogeneic or autologous. In allogeneic transplantation, progenitor cells are obtained from a donor other than the patient. For this reason, there is a need to find a suitable donor for successful treatment. As well, progenitor cells to be used can be obtained from the same individual (patient). This is referred to as autologous hematopoietic progenitor cell transplantation.
In a case where the right donor has to be found, then HLA typing is first performed on the blood samples. This method has proved effective for finding HLA-matching siblings (related donors) who can donate.
In a case where a related donor cannot be found, this method is also used to find an unrelated donor. Using oligonucleotide probes, scientists have also been able to increase the precision of HLA typing as well as matching molecule alleles for the purposes of identifying the right donors.
* While allogeneic transplantation allows for cells obtained from other donors to be used, autologous transplantation is more advantageous because of the highly reduced likelihood of morbidity and mortality. However, this type of transplantation has also been associated with the likelihood of tumor cell contamination.
Step 2: Collection of progenitor cells
The method of cell collection/harvesting varies depending on the location of these cells. In autologous transplantation, patients are first given medication to increase the production of progenitor cells into the bloodstream.
For instance, a Plerixafor injection (Mozobil) is given for a few days to mobilize progenitor cells into the bloodstream where they can be easily collected through venepuncture.
Apart from collecting these progenitor cells from circulation, bone marrow is directly collected through aspirations from the posterior-superior iliac crest. Here, the patient has to be put under anesthesia for the bone marrow to be collected multiple times.
Although this is one of the methods that can be used to collect progenitor cells, it's a rare procedure as collecting these cells from peripheral blood is much easier and effective.
Step 3: Modification
As a result of several disadvantages associated with both allogeneic and autologous transplantation, the sample has to undergo modifications in preparation for transplantation.
This may involve:
· Removal of T cells - This is particularly important in a case where the sample (bone marrow) is obtained from a different donor
· Removal of any tumor cells which may be present in autologous samples
Step 4: Preparative phase/conditioning regimen
In this step, the patient may first need to receive a high dose of chemotherapy or radiation therapy. This is carried out for a period of between one (1) and ten (10) days depending on the patient in order to destroy the disease (e.g. destroy tumor cells).
* Such treatment options as the use of serotonin antagonists help in the management of the toxicities associated with chemotherapy and irradiation.
Step 5: Transplant
The last step of transplantation involves infusing the cells. This is typically carried out a few days after the preparative step and may involve reinfusing the bone marrow with peripheral blood that contains the progenitor cells. This step is not complicated and is similar to a typical blood transfusion routine, taking between 30 to 60 minutes.
* Following the transplant phase, the patients have to be looked after as infections or complications may arise. The recovery time may take between two and three weeks before the patient fully recovers. Here, some complications may require further treatment.
As is the case with a normal, healthy individual, hematopoietic progenitor cells will gradually start to proliferate and differentiate to produce mature, functional cells depending on the needs of the body.
This process is also regulated so that the normal range of different types of cells is maintained. In the first few weeks or months, the individual may feel tired or nauseated, etc, but will likely fully recover in a couple of months.
According to some studies, hematopoietic progenitor cells found in circulation have been found to also consist of pluripotent stem cells. These cells are not only involved in the hematopoietic process but also capable of self-renewal. This is particularly important in that it allows for the retention of pluripotent stem cells that can continue giving rise to new functional cells following transplantation.
As mentioned, one of the main steps of transplantation involves mobilizing these cells from marrow sites into circulation. This is because the normal amount of progenitor cells in circulation is extremely low. Even after mobilization into circulation, a sufficient amount of blood may have to be collected several times to get the right amount of hematopoietic progenitor cells.
Apart from such medications as bolus cyclophosphamide used during recovery, treatment with drugs like recombinant human granulocyte-colony stimulating factor, etc are also used during the recovery phase to enhance the proliferation of hematopoietic stem and progenitor cells.
* To collect progenitor cells from the peripheral blood, whole blood goes through a single or multiple continuous-flow apheresis. During the recovery phase, this also involves the use of cytokine treatment.
* Following myeloablative treatment, the recommended progenitor cell dose is about 3x106 CD34+ cells per kilo of the recipient's body weight.
Following transfusion of the transplant (stem and progenitor cells), engraftment occurs where the stem and progenitor cells enter the blood. A good number of these cells have been shown to migrate to the bone marrow where they are involved in the hematopoietic process.
Depending on the patient and cells, it may take between 2 and 6 weeks for these cells to start producing new blood cells. Although it takes several weeks for the hematopoietic stem and progenitor cells to start producing new blood cells, it may take several months for an individual to fully recover from the treatment process.
Cell Markers
Cell markers may include lipids and proteins etc. These are important molecules on the surface of cells that make it possible to identify different types of cells. These molecules are also known as cell surface antigens.
Like hematopoietic stem cells, hematopoietic progenitor cells also have markers that make it possible to distinguish between the different progenitor cells.
The following are different types of hematopoietic progenitor cells and their respective markers:
· Hematopoietic multipotent progenitors: CD34+, CD38, CD45RA, and CD90
· Lymphoid progenitor cells: CD34+, CD38, CD90, and CD45RA
· Myeloid progenitor cells: CD34+, CD38, and CD45RA
· MEP (Megakaryocyte-Erythroid Progenitor): CD34, CD38, CD45RA
· Common Lymphoid progenitor cells: CD34+, CD38, CD90, and loCD45RA+
· Granulocyte Macrophage Progenitor: CD34+, CD38+, and CD45RA+
Learn more about Cell Culture, Cell Division, Cell Differentiation and Cell Staining.
See also: Neural Progenitor Cells, Endothelial Progenitor Cells
Return to Progenitor Cells main page
Return to learning about Red Blood Cells/Erythrocytes
Return to Stem Cells main page
Return to Mesenchymal Stem Cells
Return from hematopoietic Progenitor Cells to MicroscopeMaster home
References
Jennifer L. Granick, Scott I. Simon, and Dori L. Borjesson. (2012). Hematopoietic Stem and Progenitor Cells as Effectors in Innate Immunity.
Ji Yoon Lee & Seok-Ho Hong. (2019). Hematopoietic Stem Cells and Their Roles in Tissue Regeneration.
Jun Seita and Irving L. Weissman. (2011). Hematopoietic Stem Cell: Self-renewal versus Differentiation.
Reenam S. Khan and Philip N. Newsome. (2019). A Comparison of Phenotypic and Functional Properties of Mesenchymal Stromal Cells and Multipotent Adult Progenitor Cells.
Sha Hao, Chen Chen, and Tao Cheng. (2016). Cell cycle regulation of hematopoietic stem or progenitor cells.
Links
Find out how to advertise on MicroscopeMaster!