Enterococcus Bacteria
** Classification, in Urine, in Blood and Water
Classification
Domain: Bacteria
Phylum: Firmicutes (Also known as Bacillota) - Gram-positive bacteria characterized by low G+C and a rigid cell wall.
Class: Bacilli - Consists of Gram-positive bacteria. The class Bacillis is divided into two main orders namely Bacillales and Lactobacillales.
Order: Lactobacillales - Members of this order are characterized by low G+C content, and do not produce spores. They are also Gram-positive and acid-tolerant.
Family: Enterococcaceae - Gram-positive species some of which are normal inhabitants of the gastrointestinal tract (in mammals and birds).
Genus: Enterococcus - Some of the most common species in this genus are Enterococcus faecium and Enterococcus faecalis.
The genus Enterococcus consists of catalase-negative, Gram-positive bacteria. Members of this group are facultative anaerobes and thus can be found in different habitats including the soil, oral cavity, and large intestine of human beings and other mammals, and sewage.
They can also tolerate varying environmental conditions such as temperature range of between 10 and 45 degrees C and pH range of between 4.5 and 10.0.
Other members of the genus Enterococcus include:
- Enterococcus aquimarinus
- Enterococcus avium
- Enterococcus canis
- Enterococcus ratti
- Enterococcus dispar
- Enterococcus caccae
General Characteristics of Enterococcus
Morphology
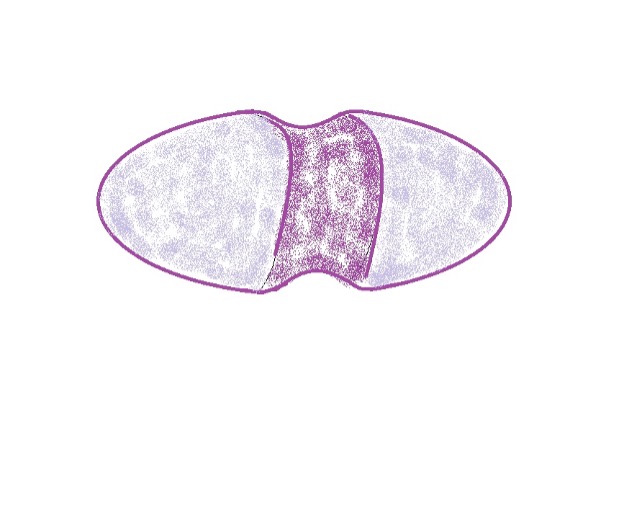
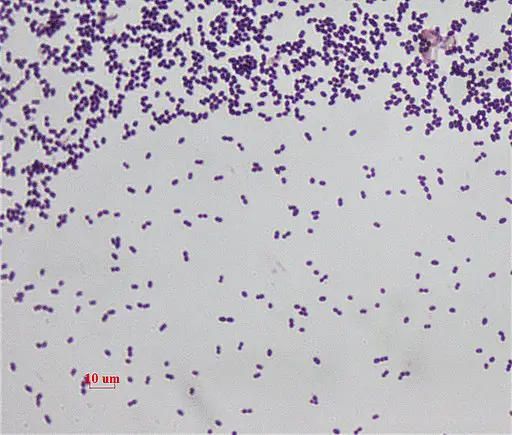
Enterococcus bacteria are spherical or ovoid in shape and occur in pairs (or short chains). They measure between 0.6 and 2.0 um in length and motile species move by means of terminal flagella.
They do not produce spores.
There are about 18 described species.
As facultative anaerobes, they can grow in aerobic and anaerobic conditions (given other environmental conditions are favorable).
They are opportunistic pathogens and can cause a number of infections including meningitis, diverticulitis, bacteremia, and urinary tract infections.
Enterococcus Bacteria in Urine
Urinary tract infections caused by certain Enterococcus species have been shown to be on the increase, especially among hospitalized patients. According to Webmd, these species are responsible for about 110,000 cases of urinary tract infections in the United States each year.
Urinary tract infection (UTI) refers to an infection of any part of the urinary system (e.g. urethra, kidneys, and ureter). Like E. coli, and Proteus mirabilis, Enterococcus faecalis is one of the most common causes of this infection.
While some of the infections tend to be mild (uncomplicated), others are serious (complicated) and can result in the obstruction of the urinary tract, urine retention, renal failure, and even compromised pregnancy.
As mentioned, most of the infections caused by Enterococcus occur in hospital settings. In the United States, as many as 80 percent of UTIs are attributed to indwelling catheters.
* Unlike E. coli, Enterococcus faecalis is largely associated with uncomplicated urinary tract infections. However, it's worth noting that the bacterium can also cause complications in certain cases.
Mechanism of Infection
From the Gut to the Urinary System
As ubiquitous organisms, Enterococcus bacteria can also be found in various food materials and are therefore considered contaminants. However, they can also be beneficial in that they are involved in the ripening of various foods as well as producing desired flavor characteristics in cheeses through processes like lipolysis and citrate breakdown.
For this reason, they are some of the most common microbes in the gastrointestinal tract where they exist as commensals. Some of the strains are characterized by several virulence factors that increase the capacity to cause disease or aggravate existing symptoms.
Here, one of the most important features is the presence of surface proteins that promote adherence and colonization. This is an important trait that makes it possible for the bacterium to invade the urinary system.
Using pili and adhesions (surface proteins like Ebp pili and Ace adhesin used for adhesion), Enterococcus faecalis has been shown to be capable of migrating and contaminating the periurethral area and colonizing the urethra. From here, they can also migrate to the bladder and gradually colonize the superficial umbrella cells.
Catheter Implantation
While Enterococcus bacteria can migrate to the urinary tract from the gut, infections during catheter implantation are also very common. The infections can result in bladder inflammation as well as the accumulation of fibrinogen into the catheter.
Using fibrinogen as a source of energy, they can proliferate and spread to other parts of the urinary system. Moreover, they have been shown to use fibrinogen to form biofilms which protect them from cells of the immune system.
* For the most part, Enterococcus species use Ebp pili (endocarditis- and biofilm-associated) in catheter-associated urinary tract infections (CAUTIs). The pili are also responsible for persistent infections.
Along with the mechanical stress caused by the catheterization process, these bacteria can end up causing edema, kidney lesions, and exfoliation of the uroepithelium.
* Enterococcus cannot grow in urine.
* Enterococcus have also been shown to be resistant to a number of antimicrobials. For instance, Enterococcus faecium is resistant to aminoglycodies like gentamicin and streptomycin.
* Enterococcus are responsible for 15 to 20 percent of urinary tract infections identified in hospital settings.
Enterococcus in Blood
Based on studies published in the mid-2000s, Enterococcus bacteria were shown to be some of the most common causes of nosocomial bloodstream infections. In the United States, for instance, the bacteria was found to be the third most common cause and the fourth in Denmark.
Overall, mortality rates as a result of these infections (bacteremia) were shown to range between 19 and 48 percent. Though it was previously thought that most of the deaths occurred among patients with underlying illnesses, similar figures were reported among patients without such illnesses.
* Enterococcus can enter the bloodstream through a number of routes. These include intravenous lines, translocation from the urinary tract and gastrointestinal tract, as well as wounds. Of these, catheter-associated UTIs (urinary tract infection) has been shown to be the most common route.
Translocation of these bacteria from the gut is often the result of overgrowth (overgrowth in the gut and particularly the colon). Aside from migrating into the bloodstream under certain conditions, studies are finding that there are various mechanisms that contribute to the translocation. One, in particular, involves transportation by phagocytic cells.
In this case, enterococcus is first phagocytized by given phagocytic cells (e.g. dendritic cells, tissue-resident leukocytes, or intestinal epithelial cells). They are then transported across the intestinal wall to underlying lymph nodes where they are filtered out.
In cases where they are not destroyed by phagocytic cells, the bacteria can cause abscesses in the reticuloendothelial organ which in turn allows systemic spread.
* Enterococcus faecalis is capable of surviving in peritoneal macrophages for about 72 hours. This increases the chances of the systemic spread.
In another study where overgrowth of the bacterium (Enterococcus faecalis) was induced using antibiotic treatment, it responded by increasingly adhering to the walls of the caecum, colon, and ileum followed by migration into the spleen, lymph nodes, and liver. This demonstrated the ability of the bacterium to migrate from the gut into the bloodstream.
Apart from translocation through adherence, Enterococcus can also gain entry into the bloodstream through diffusion. In this case, the bacteria, like a number of other inert particles, penetrate the mucosal barrier to reach the bloodstream.
While they are likely to be ingested by phagocytic cells, the fact that they can survive within these cells for up to 72 hours increases the chances of successful translocation.
Bacteremia
Bacteremia refers to the presence of bacteria in the bloodstream (in circulating blood). In studies involving mice, Enterococcus faecalis was also found to cause lysis of neutrophils and macrophages in blood. This not only allowed the bacteria to thrive but also successfully spread to and colonize distant organs such as the heart. Though Enterococcus bacteria (especially E. faecalis) is suspected to produce a number of toxins, the cytolysin toxin streptolysin might be responsible for the lysis of target cells (macrophages, red cells, and polymorphonuclear neutrophils). In a number of culture studies, the toxin was reported to cause hemolysis in blood agar.
In cases where the bacterium reaches the heart through circulating blood, it can cause infective endocarditis (IE), particularly among older men. Using adhesive features (aggregation substances like surface proteins), the bacterium adheres to the endocardium where they not only form a biofilm-like matrix but also continue to proliferate.
One of the biggest benefits of this matrix (for the bacterium) is that it makes it difficult for antibiotics and immune cells to penetrate. This protects the organisms from the body's immune system.
* Some of the proteins involved in cell-to-cell adhesion are Asp, Asa1, and Asc10.
In non-bacterial thrombotic endocarditis (NBTE), damage to the endocardial lining might be caused by the turbulent flow of blood. This exposes the underlying collagen tissue factor and induces the adhesion of fibrin and platelets.
As a result, a blood clot (thrombosis) might be formed. If bacteria like Enterococcus faecalis move to the heart and come in contact with the clot, they can adhere (using adhesins) and cause an infection (vegetation).
* Enterococcus biofilm-like matrix in the heart usually forms in areas of low pressure. For this reason, they are likely to be found at the aortic and mitral valves.
This vegetation can activate increased production and accumulation of immune cells (e.g. neutrophils and macrophages) against the infection. In turn, this may activate the secretion of cytokines which can start eroding the perivalvular tissue. The infection is thus associated with a number of negative impacts on the heart including dysfunctional heart valves, congestive heart failure, and conduction problems.
If pieces of the bacterial vegetation break apart into smaller pieces, they can form emboli which can block arteries. On the right side of the heart, the emboli can be transported to the lungs causing pulmonary infarction and respiratory symptoms.
If this occurs on the left side, then the emboli can be transported to the other organs in the body where they can interfere with blood supply and nourishment.
Symptoms
Some of the most common symptoms include:
Fever - Secretion of IL-1, IL-6, and TNF-alpha stimulates the release of prostaglandin e2 in order to increase body temperature. This is aimed at affecting bacterial growth and also results in a fever.
Leukocytosis - The infection induces increased production of white blood cells to fight the bacteria.
Pulmonary edema and hypotension - Caused by accumulation of blood in the left ventricle: This is often a result of affected valve activities (mitral valve).
Enterococcus in Water
Enterococcus can be found in seawater, wastewater (hospital water and sewage), and surface water. Because they are commonly found in the gut of human beings and some animals, they are commonly used as fecal indicator bacteria to indicate contamination in the environment. That said, it's worth noting that based on many research studies, the presence of these bacteria in various habitats may not be the result of human and animal input.
Some of the habitats in which the bacteria may naturally exist (extraenteric habitats) include beach sand, ambient water, soil, and some aquatic vegetation.
As mentioned, Enterococcus are ubiquitous organisms. As such, they can be found in different habitats across the globe. This is attributed to the fact that they can survive under varying environmental conditions.
One of the main characteristics of the Enterococcus bacteria is that they can survive in habitats with relatively high salt concentrations (6.5% NaCl). As such, they can thrive in marine waters much better as compared to some of the other gut microorganisms.
A number of other factors like oxygen content in these habitats can have a negative impact on bacterial growth. For this reason, survival and proliferation are also dependent on other factors in this environment.
* The fact that they can better tolerate higher salt concentration qualifies them as better indicators of human health risks in marine recreational waters.
* Some studies have revealed an inverse relationship between salinity and enterococci concentration. In higher salt concentrations, some of the species are incapable of proliferation.
- In these studies, these organisms were found to survive longer in freshwater as compared to salt water. Some researchers have attributed this decline (of Enterococci in salty water) to the predation activities of protozoa.
Apart from factors like oxygen content, the survival and proliferation of the bacteria can also be affected by nutrient availability. As compared to other environments/habitats, the gastrointestinal tract is nutrient-rich and thus supports proliferation. Therefore, the bacteria face the risk of starvation when they are released into oligotrophic aquatic habitats.
Based on several studies, Enterococcus faecalis has been shown to survive longer in sterilized sewage as compared to sterilized lakes among other bodies.
Compared to sterile lakes, sterilized sewage contains more organic material that can support life. This indicates the significance of nutrition for the bacteria in aquatic environments.
Some of the aquatic environments/habitats in which Enterococcus bacteria have been shown to exhibit persistent growth and proliferation include:
Aquatic Habitats with Vegetation
Availability of nutrition is one of the most important factors for the survival of an organism. In various marine and freshwater environments, the green alga Cladophora has been shown to support the growth of various Enterococcus species among other microorganisms.
Along the shorelines of Lake Michigan, for instance, the alga supports a number of bacteria including Enterococcus, Shigella, and E. coli. In studies where the algal mats were sundried and stored at 4 degrees C, Enterococcus survived for over 6 months and even began to grow and proliferate when the mats were rehydrated.
Aside from Cladophora, these enterococci can also survive and grow in the presence of decaying seaweed and flowing plants of various plants.
Beach Sand
A number of Enterococcus bacteria species are suspected to be natural residents of various beach sands across the globe. These include Enterococcus hirae, Enterococcus mundtii, Enterococcus durans, and Enterococcus casseliflavus.
Although desiccation affects growth, transient growth has been reported when the sand becomes wet which shows that the bacteria can survive for a period of time under unfavorable conditions.
While some of the species may occur naturally in this habitat, others like Enterococcus faecalis and Enterococcus faecium are introduced by birds (e.g. geese and gulls) and even human beings who visit these beaches
Sediments
Various Enterococcus species can be found in marine and freshwater sediments. More importantly, these habitats have been shown to be the most significant reservoirs/sources of the bacteria. As compared to the populations found in other habitats (aside from the gut), these habitats contain higher populations which might be attributed to better overall conditions. Moreover, species in these habitats are suggested to exhibit better resistance to a range of stressors including solar inactivation and predation.
The close interaction with surface water also improves the general conditions that the organism need for survival. For instance, water contains a variety of organic material for nutrition and also allow the bacteria the opportunity to change habitats with changing environmental conditions.
Moist Soil
Most of the Enterococcus bacteria species found in soil survive longer during spring and winter than in the summer. Although they are more ubiquitous in soil than some of the other microbes (e.g. E. coli), they are likely to be found in higher concentrations in moist and less-impacted soils.
They also have greater survival abilities as compared to various Gram-negative bacteria which might explain why they survive longer in the soil.
Return to Bacteria - Size, Shape and Arrangement
Return to Hydrogen-Oxidizing Bacteria
Return from Enterococcus Bacteria to Diplococci Bacteria
Return to MicroscopeMaster home
References
Byappanahalli, M. et al. (2012). Enterococci in the Environment.
Mireles, A., Walker, J., Caparon, M., and Hultgren, S. (2015). Urinary tract infections: epidemiology, mechanisms of infection and treatment options.
Tyne, D., Martin, M., and Gilmore, M. (2013). Structure, Function, and Biology of the Enterococcus faecalis Cytolysin.
Selleck, E., Tyne, D., and Gilmore, M. (2019). Pathogenicity of Enterococci.
Links
https://www.sciencedirect.com/topics/engineering/enterococci
https://www.sciencedirect.com/topics/immunology-and-microbiology/enterococcus
Find out how to advertise on MicroscopeMaster!