Diplococci Bacteria
Definition, Shape, Examples, Diseases/Treatment
Definition
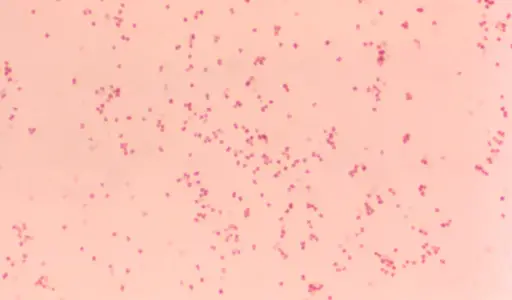
Essentially, diplococci bacteria (singular; diplococcus) are rounded/spherical bacteria that occur in pairs. Unlike staphylococci bacteria (which form grape-like clusters and are truly round), some may appear ovoid (elongated) or bean-shaped.
There are both Gram-positive and Gram-negative bacteria that are responsible for various infections in human beings.
Some examples of diplococci bacteria include:
- Moraxella species
- Neisseria spp - e.g. Neisseria cinerea and Neisseria gonorrhea
- Streptococcus pneumoniae - usually occur in pairs
- Enterococcus - some species occur in pairs (while others form short chains)
Shape
As mentioned, diplococci bacteria may appear rounded or elongated in shape. As such, some species may not be truly round as is the case with staphylococci bacteria. As such, they are often described as having an ovococcoid shape.
Based on various studies, this shape is attributed to two distinct peptidoglycan machineries. For coccoids (truly round bacteria) like Staphylococcus aureus and micrococcus, the cell division machinery is responsible for the synthesis of septal peptidoglycan and thus the growth of the cell wall.
For ovococcoid bacteria, like some diplococci, synthesis of the cell wall occurs through the cell division machinery that is responsible for synthesis of the septal peptidoglycan and the elongation complex responsible for the peripheral peptidoglycan.
Here, it's worth noting that unlike most eukaryotic cells that tend to be irregular in shape, bacteria tend to have a regular shape (spherical, rod-like, etc).
For bacteria, the shape is defined and maintained by the cell wall (which consists of peptidoglycan, a cross-linked polymer). However, the mode and mechanism of division also help influence the type of shape that a given type of bacteria will have.
For Streptococcus pneumoniae, as is the case with the other diplococci bacteria, division occurs in the parallel plane perpendicular to the long axis.
During cell division, the site of division is first marked by the equatorial ring (also known as the wall band). Here, studies have shown the process to be mediated by FtsZ, a tubulin homolog that produces dynamic filaments in the middle of the cell.
Following the polymerization of these filaments, binding of a series of proteins is initiated which in turn promotes the synthesis of septal peptidoglycan as the cell divides. This process is also characterized by the splitting of the equatorial ring into two.
Here, the ring splits into two equal rings once the cell starts dividing and consequently delimits a zone for peripheral peptidoglycan synthesis. At the same time, the identical rings continue moving from the center to become markers of cell division for the identical daughter cells.
* The septal peptidoglycan synthesis is mediated by a number of proteins that include class B proteins (bPBP2x). As they close inside, these proteins play an important role of separating the daughter cells.
Unlike septal peptidoglycan synthesis, peripheral PG synthesis is regulated by a number of proteins including bPBP2b. As they emanate from the mid-cell outwards, these products gradually elongate the cells causing them to become ovoid in shape.
* In the event of incomplete cell division, studies have shown ovococci bacteria to develop chains or filaments.
Gram Positive Diplococci Bacteria
Two of the most common Gram-positive diplococcus includes Streptococcus pneumoniae and Enterococcus species. Normally, Streptococcus pneumoniae lives as a commensal in the mucosal surfaces of the respiratory system in human beings. However, it can cause community-acquired pneumonia under certain conditions (it's an opportunistic pathogen).
Enterococcus species, on the other hand, are normal intestinal flora of human beings and animals. While they are commonly found in the gut and bowel, they can also be found in the mouth.
Despite their differences, Streptococcus and Enterococcus bacteria share the same morphological characteristics thus making it difficult to differentiate the two based on morphology.
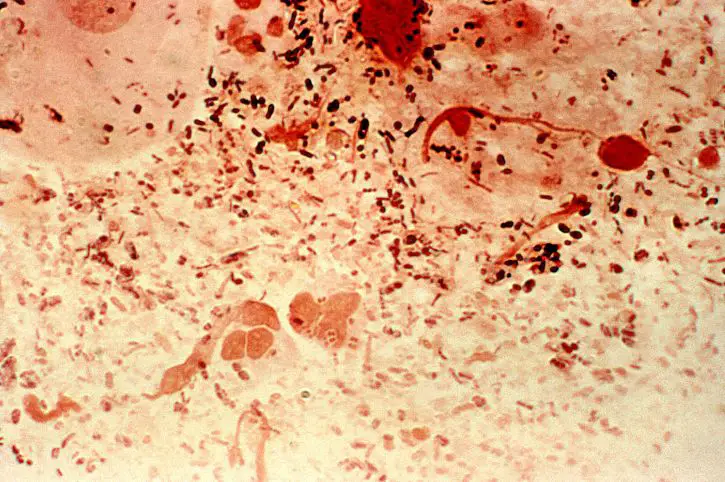
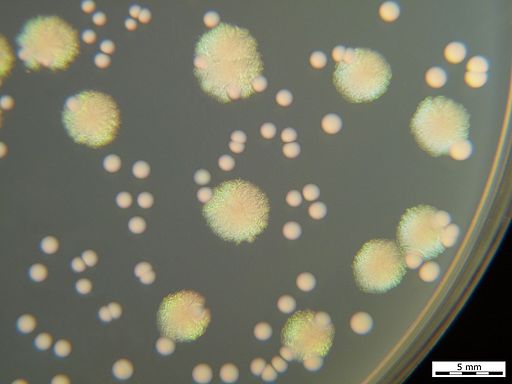
Using Gram stain, it's possible to differentiate between Gram-positive and Gram-negative diplococci. Before Gram stain, the bacteria can be grown in culture in order to increase their numbers or study their characteristics in culture.
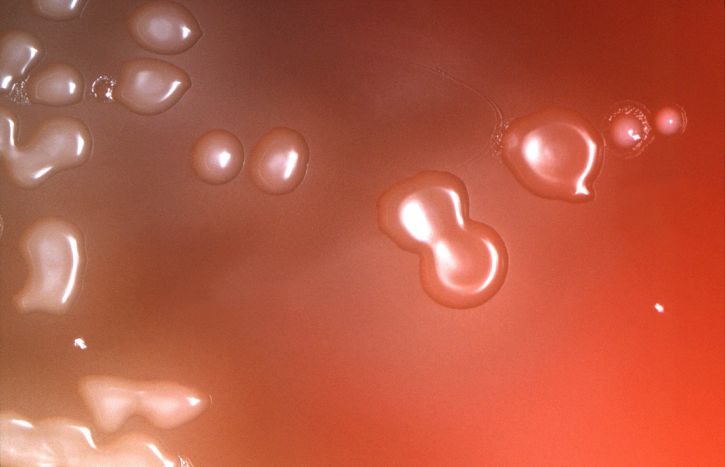
* Being a fastidious bacterium (requires complex nutrition); Streptococcus pneumoniae can be grown in culture that contains blood or chocolate agar. Some of the conditions required for growth include 5 percent carbon dioxide and 35 to 37 degrees C.
Enterococcus bacteria can be grown in Bile Esculin Agar where they hydrolyze esculin to produce glucose and esculetin.
See more on Gram positive and Gram negative bacteria.
Requirements for Gram stain
- Sample - specimen from culture can be used
- Gram stain reagents
- Bunsen burner
- Glass slides
- Staining rack
- Water
Procedure
· Place a small amount of the specimen on the glass slide at the center of the glass slide and create a thin smear - a sterile wire-loop can be used
· Allow the slide to air-dry and then heat fix for a few seconds making sure not to overheat
· Flood the slide with crystal violet and let it stand for about 1 minute
· Gently wash the slide with clean tap water for a few seconds
· Flood the slide with Gram's Iodine (the mordant) and allow it to stand for about 1 minute and then gently wash with water for a few seconds
· Add a few drops of the decolorizer (the decolorizing agent commonly used is ethyl alcohol or acetone) until it runs clear
· Flood the slide with the counterstain (Safranin) and allow it to stand for between 30 seconds and 1 minute and then gently wash with clean water
· Observe the slide under the microscope under oil immersion
Observation
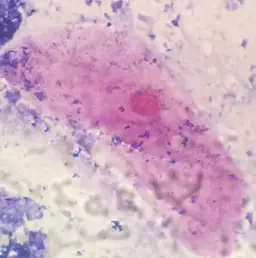
When viewed under the microscope, Streptococcus pneumoniae is often seen in pairs. However, it's also possible to identify single cells or short chains. Generally, they are elongated and may have slightly pointed ends. They also appear purple in color which indicates that they are Gram-positive bacteria (having retained the primary stain).
Like Streptococcus pneumoniae, Enterococcus species can also be seen in pairs, but can also form short chains. They are also purple in color when viewed under the microscope indicating that they are Gram-positive diplococcus.
* As mentioned, there are both Gram-positive and Gram-negative diplococcus bacteria. Gram-negative diplococci like Moraxella catarrhalis will appear pale pink in color.
* As compared to Gram-negative diplococci, Gram-positive diplococci have a thicker peptidoglycan layer (between 20 to 80nm thick). As such, it retains the primary stain even after decolorization
Diseases
As mentioned, there are several types of bacteria that are classified as diplococci bacteria given that they occur in pairs.
This section will focus on four types of diplococci bacteria and some of the diseases they cause.
Neisseria
Neisseria is a large genus that consists of organisms that normally colonize the mucosal surface of animals.
Two of the species responsible for human diseases include:
Neisseria Gonorrhoeae
Also known as gonococcus, Neisseria gonorrhoeae is a Gram-negative bacterium that does not form spores. It's an obligate human pathogen that is sexually transmitted in human beings.
Following transmission of the bacteria from an infected individual, it uses pili (protein appendages located on the cell wall) as well as opa proteins (opacity proteins/protein II) to adhere to the columnar epithelial cells which makes it easier for them to penetrate the cells.
Based on studies, gonococci adhesion has been shown to be one of the most important steps with regards to pathogenesis of the organism. Following penetration, the bacteria proliferates in the basement membrane which allows them to increase in numbers and infect new cells. In some cases, the bacteria can be spread through the bloodstream to other parts of the body.
* Given that gonorrheal infections are, for the most part, limited to mucosal surfaces that consist of columnar epithelia, the infections are common in the urethra, pharynx, conjunctiva, and rectum.
* A gonorrheal infection is typically characterized by a scanty, cloudy, or clear discharge. For this reason, infections caused by Neisseria gonorrhoeae are also referred to as purulent infections. The infection may also cause dysuria - painful urination.
Treatment - Currently, gonococcal infections are treated using a number of antimicrobial agents including ciprofloxacin, ceftriaxone, and oflaxacin. Here, drugs are used to prevent attachment and entry of the pathogen into the host cells.
Neisseria Meningitidis
Like Neisseria gonorrhoeae, Neisseria meningitidis (meningococcus) is a Gram-negative bacterium. In human beings, the bacteria is responsible for several diseases/infections including meningococcal disease and life-threatening sepsis. Infections have been shown to result from aspiration of the infective organism or through contamination by blood or other bodily fluids.
In the body, the bacterium first attaches to the epithelial cells (e.g. in the nasopharyngeal mucosa) and consequently crosses the mucosal barrier in order to enter the bloodstream. There are several factors that contribute to pathogenesis of the bacteria include adhesive proteins, a capsule, as well as several other molecules.
For the capsulated N. meningitidis, the capsule allows them to evade the antibody and phagocytic activities of phagocytes. The Lipopolysaccharide and adhesins like pili and opacity proteins (Opa proteins) allow the bacteria to adhere to the epithelium. If not cleared early, the bacteria enters the bloodstream where they are transported to the central nervous system.
Here, the bacteria can cause meningitis (infection of the fluid that surrounds the meninges) particularly among individuals who lack antibodies that target capsular/noncapsular antigens associated with invading serotypes. Meningitis in human beings is characterized by stiffness of the neck, fatigue, and vomiting, etc.
Treatment - Generally, acute bacterial meningitis is treated using antibiotics (intravenous antibiotics), penicillin, and corticosteroids in some cases.
Moraxella
Named after Victor Morax, a Swiss ophthalmologist, Moraxella is a genus of Gram-negative bacteria that belongs to the family Moraxellaceae. While some of the species are characterized by a rod-like morphology, some occur in pairs and are classified as diplococci. Moraxella catarrhalis is one of the most common species of the genus Moraxella.
Like some of the other diplococci bacteria, Moraxella catarrhalis is a Gram-negative diplococcus bacterium. It's also fastidious and non-motile and the causative agent for several infections in different parts of the body. Generally, the bacteria is a member of the normal flora that inhabits the mucous membrane.
While Moraxella catarrhalis can be found in adults, many studies have shown that the bacteria often colonize the respiratory system (the upper respiratory system) early on in life (during the first year of life). For this reason, it's commonly found among school-going children (40 to 50 percent of school-going children). Here, transmission is largely as a result of direct contact with droplets from an infected individual.
As is the case with some of the other diplococci bacteria, Moraxella catarrhalis have been shown to possess lipopolysaccharide, surface proteins, and pili that allow then to adhere to epithelial cells of the upper respiratory system.
Following attachment (adhering) to these cells, in vitro studies have shown the bacteria to invade the cells. This is particularly important for the pathogen allowing them to evade the host immune system.
Some of diseases/infections caused by the bacterium include:
Otitis media - In children and infants, Moraxella catarrhalis is the main cause of otitis media. Here, studies have shown the pathogen to migrate from the upper respiratory tract to the middle ear through the eustachian. The infection is characterized by congestion of the eustachian tube due to inflammation. As a result of this congestion, individuals are likely to experience a negative pressure in the middle ear
* In the case of otitis caused by Moraxella catarrhalis, treatment options include Amoxicilin-clavulanate and trimethoprim-sulfamethoxazole among others.
Sinusitis - While Moraxella catarrhalis is considered part of normal flora in the respiratory system (particularly the upper respiratory system), it can cause sinusitis (acute sinusitis) in children.
Essentially, sinusitis refers to the inflammation of the tissue that lines the sinuses. The infection is characterized by nasal discharge and cough for a period of about 10 days.
Depending on the person, the bacteria may also migrate from the nasopharynx to the adjacent sinuses where favorable conditions allow it to proliferate. In a case where the mucociliar clearance mechanism is disturbed, studies have also shown there to be fluid retention which in turn results in increased discharge.
In children and some adults, the bacteria has been shown to cause about 20 percent of all cases of acute bacterial sinusitis.
* Treatment - Currently, treatment of acute sinusitis caused by Moraxella catarrhalis include a high dose of amoxicillin and macrolides for some patients.
Pneumonia and bronchitis - While M. catarrhalis-related pneumonia is not common, it has been reported in some elderly patients with cardiopulmonary disease as well as those with a compromised immune system. The bacteria is associated with an increased risk of bronchiolitis in the early years of life.
Streptococcus Pneumoniae
As mentioned, Streptococcus pneumoniae is commonly found in the mucosal surfaces of the nose and throat where they live as commensalism. Like some of the other diplococci, Streptococcus pneumoniae is characterized by surrounding capsule as well as type I pili that promotes interaction with host cells.
In human beings, pneumococcal pneumonia is one of the main diseases caused by the bacterium. The bacteria is mostly spread through coughing (respiratory droplets) and migrates to the upper respiratory tract before reaching the lungs.
Following an incubation period of 1 to 3 days, some of the clinical symptoms associated with the infection may include abrupt fever and chills, chest pains, rusty sputum, and hypoxia among others.
An infection in the upper respiratory tract can also spread to the nervous system through the blood causing pneumococcal meningitis. This is a life-threatening infection characterized by seizures, fever and headache, lethargy, nuchal rigidity, and coma, etc. Spread of the bacteria to the bloodstream can also result in bacteremia and the consequent sepsis.
* Treatment - In the case of outpatient pneumonia, treatment options include such antibiotics as amoxicillin and macrodine among others. On the other hand, intravenous ampicillin and ceftiaxone and commonly used for inpatient pneumonia. Pneumococcal meningitis is commonly treated with penicillin, cefotaxine, and ceftiaxine.
Enterococcus
Enterococcus faecium is one of the most common species of the genus Enterococcus. Like some of the other diplococci, Enterococcus faecium is a commensal that co-exist with the host (human beings) without causing harm.
In humans, the organism can be found in the gastrointestinal tract where it can cause diseases under given conditions. Using enterococcoal surface proteins, the bacterium is able to form biofilms which, along with such virulence factors as gelantinase, makes it more resistant to antibiotics particularly when compared to E. faecalis.
The bacterium has been associated with a number of diseases/infections including endocarditis and neonatal meningitis. While Enterococcus faecium is not a common cause of bacterial meningitis, it's associated with a high mortality rate due to the virulence factors that make it resistant to various antibiotics.
Treatment - Currently, treatment options for enterococcal meningitis involves a combination of ampicillin and streptomycin or gentamicin. Here, however, it's worth noting that for the most part, Enterococcus species responsible for various infections tend to be resistant to a wide range of antibiotics. For this reason, a combination of drugs are used for different infections/diseases depending on the level of infection.
See also: How do antibiotics kill bacteria?
Return to Bacteria - Size, Shape and Arrangement
More on Bacteria under the Microscope
Return from Diplococci bacteria to MicroscopeMaster home
References
Ann C. Smith and Marise A. Hussey. (2005). Gram Stain Protocols.
Ellie J.C. Goldstein, Timothy F. Murphy, and G. Iyer Parameswaran. (2009). Moraxella catarrhalis, a Human Respiratory Tract Pathogen.
Nela Holečková. (2015). LocZ Is a New Cell Division Protein Involved in Proper Septum Placement in Streptococcus pneumoniae.
Nelson I. Agudelo Higuita and Mark M Huycke. (2014). Enterococcal Disease, Epidemiology, and Implications for Treatment.
Omeed Sizar and Chandrashekhar G. Unakal. (2020). Gram Positive Bacteria.
Sara Bernhard, Violeta Spaniolb, and Christoph Aebi. (2012). Molecular pathogenesis of infections caused by Moraxella catarrhalis in children.
Links
Find out how to advertise on MicroscopeMaster!