Hematuria
Microscopy of Urine and Observations
Essentially, hematuria refers to the presence of blood in the urine. Clinically, a patient is found positive once it is confirmed that there are 5 or more red blood cells in a high-power field (under compound microscope) in three consecutive specimens.
Here, a patient may be asked to provide several samples that are centrifuged and viewed under the microscope. In the event that these samples are found to have 5 or more red cells under high-power field of view, then one is said to have hematuria.
There are two types of hematuria, which include:
- Gross hematuria - may appear smoky, tea-colored or bloody. As such, the patient can detect that there is blood in their urine
- Microscopic hematuria - In this case, the patient may not be able to tell that there is blood in the urine, which means that it's asymptomatic. This requires the use of a microscope.
Some of the signs associated may include:
- passage of clots in urine
- dysuria and abdominal pain
- joint pains
- skin rashes
Microscopy of Urine
Although gross hematuria can be detected without using a microscope, one can still be used to determine the severity of the condition. It's also important given that it helps confirm the presence of red blood cells in urine.
However this is not always the case, microscopic examination of urine may be performed as part of urinalysis. Generally, urinalysis is used to detect and reveal such diseases as diabetes mellitus and urinary tract infections among others. Urinalysis may include various chemical, visual and microscopic tests.
Hematuria microscopy is specifically aimed at detecting the presence (or the absence) of red blood cells in urine. However, hematuria microscopy is part of the urinalysis tests.
Requirements
- Urine sample
- Test-tube
- Centrifuge
- Compound microscope
- Glass slide and cover slip
Sample Collection
A clean, plastic container is used to collect urine for microscopy.
Here, it is often encouraged that the patient collect mid-state sample, which helps reduce chances of contamination while at the same time increasing accuracy. Basically, this means that the patient/individual should collect the urine halfway "mid-stream" rather than when they first start urinating.
While it can be stored for a period of up to 72 hours, it is often recommended that the sample be observed as soon as possible for specimen stability.

Preparation
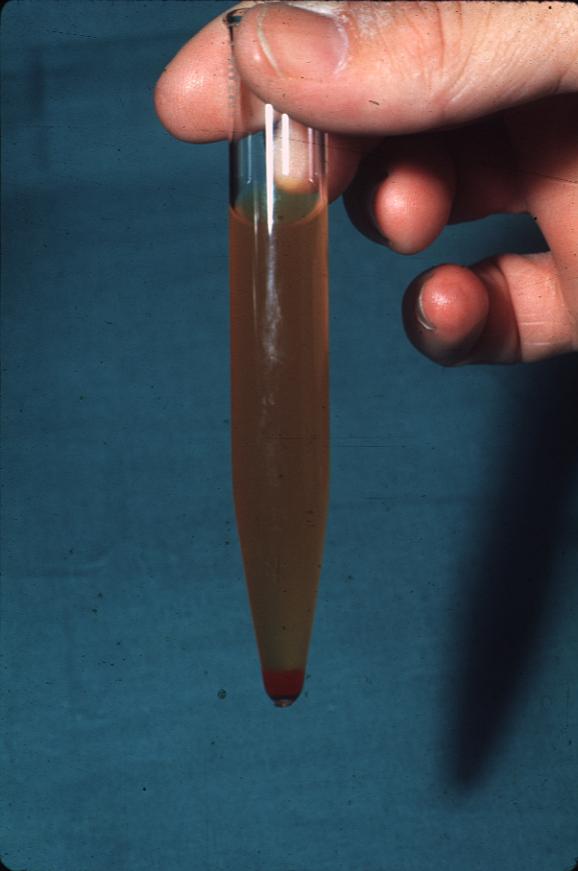
Shake the sample well and pour about 12ml of the urine into a test-tube. Insert the test-tube into a centrifuge and set the speed to between 2,000 and 3,000 rpm (rounds per minute). These are relatively low speeds. The test-tube should be left in the centrifuge for about 8 minutes until the sediment forms at the bottom. Once it is removed from the centrifuge, the sample will have separated into a supernate and the sediment.
The supernate should be decanted leaving only a very small amount of about 0.5 ml to avoid pouring out the sediment. To mix the sediment with the remaining supernate, simply flick the bottom part of the tube and pour this on to the glass-slide.
- Supernate - The supernate is the liquid that remains at the top above the solid that settles at the bottom. This separates from the denser solid at the bottom.
- Sediment - Sediments includes the matter that settles at the bottom of the test-tube. When put in a centrifuge, the rotation causes this matter which has higher density to travel to the bottom of the tube and settle thus being separated from the less dense liquid.
Shaking the sample before adding some into the test-tube is particularly important given that it allows for the contents of the sample to spread. When the sample is allowed to settle, denser components of the sample will gradually settle at the bottom, which would result in inaccurate results. Therefore it's important that the sample be shaken to ensure even distribution of urine components.
Relatively low speeds are also recommended when the sample is being centrifuged. Although high speed would mean quick results, it would also result in high pressure that may cause hemolysis (bursting of the red cells). This would also affect the accuracy of results when the sample is viewed under the microscope.
Related: Laboratory Centrifuge
Viewing Under the Microscope - Hematuria
Flicking the bottom of the test-tube helps mix the remaining contents of the test-tube and make it possible to collect the sediment. Once a drop of the sediment is placed on a clean glass slide, it should be covered with a cover slip
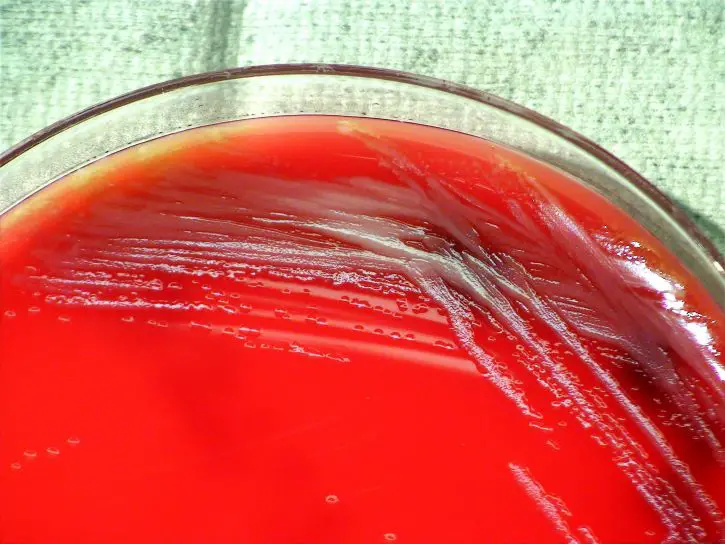
Place the slide under the microscope (compound microscope) and start with low power. Here, students will be able to view the larger components of the sample including casts and crystals.
Under high magnification, the student should be able to see (if present) the red blood cells along with any other types of cells (bacteria etc) that may be present.
* Ideally, a urine sample should not contain any red blood cells. However, due to various reasons (menstruation etc) it's possible for some of these cells to find their way into urine. This becomes a problem when 5 or more of the red cells are found in every field of view when being observed under high magnification.
Observation
When viewed under the microscope, red blood cells (in the sample) may appear to vary in shape and size.
For instance, they may appear as:
- Normally shaped
- Swollen
- Partly hemolyzed
- Crenated
The red blood cells are likely to be swollen, which is due to dilute urine. When the urine sample is very dilute, water moves into the cell through osmosis. As water from the dilute urine enters the cell, it swells and thus appears larger under the microscope.
In a hypertonic state, the red cells will become crenated, which means that they lose water and shrink. The cells will therefore be seen as notched objects under the microscope.
See also: Articles on Blood Microscopy and Blood Smear
Return from Hematuria to MicroscopeMaster Research Home
References
Roberts, James R. (2015) Urinalysis: Microscopy.
https://library.med.utah.edu/WebPath/TUTORIAL/URINE/URINE.html
https://labtestsonline.org/understanding/analytes/urinalysis/ui-exams/start/2
Find out how to advertise on MicroscopeMaster!